Eye diseases
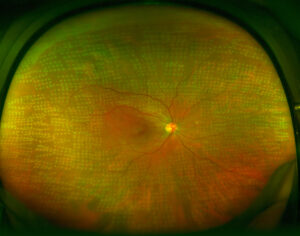
Diabetic retinopathy
What is diabetic retinopathy?
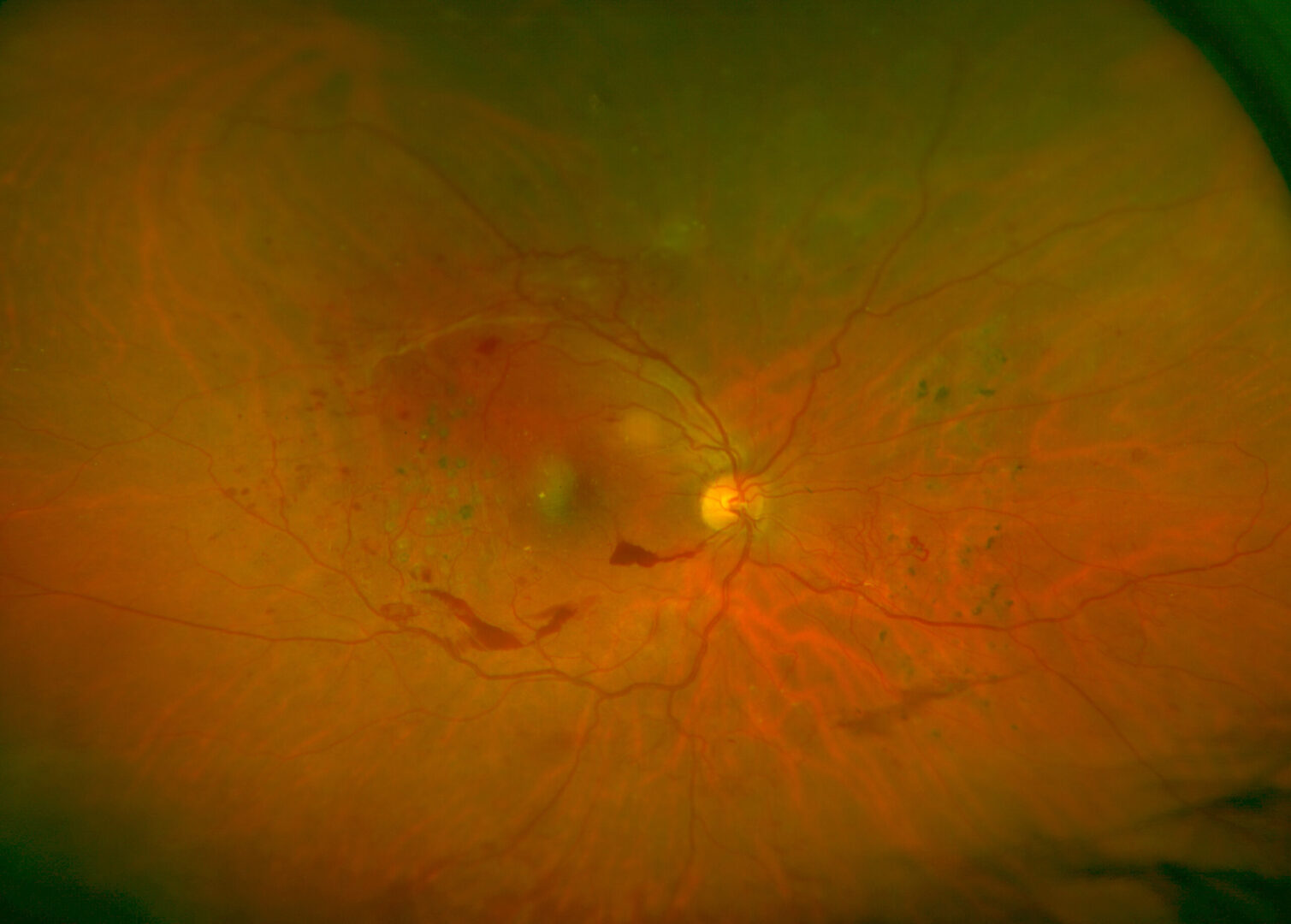
Diabetic retinopathy is a retinal disorder (layer lining the inside of the eyeball) as a result of diabetes, which affects the eye in the same way as the rest of the body, mainly altering circulation. Due to the metabolic decompensation caused by having high levels of blood sugar (glycemia), changes of varying severity may occur to the very vascularised retinal tissue. The main damage includes:
- Increased vascular permeability such that the blood vessels lose liquid. When this collects in the central portion of the retina, a macular oedema appears.
- Retinal ischemia or lack of irrigation in some parts of the retina, due to the closure of small blood vessels. This can cause the death of the cells in the macula (centre of the retina and area of greater visual acuity) as well as the appearance of new abnormal blood vessels whose growth can cause complications such as retinal detachment, vitreous haemorrhages or even very complex neovascular glaucomas.
Diabetic retinopathy is one of the leading causes of blindness in Spain although fewer and fewer patients with diabetes are suffering severe vision loss thanks to improvements in treatments and better preventive knowledge. However, despite it being known that diabetes is a severe risk factor for sight, it is estimated that 40% of diabetics have never had an ophthalmological examination.
Symptoms
Causes and risk factors
Treatment
In its early stages, diabetic retinopathy does not usually present symptoms so it is very important that if you have diabetes you have regular eye checks, as indicated by your specialist, to assess the health of your ocular fundus. This is the only way to detect possible retinal disorders early and before the damage progresses and the ocular erosion is obvious and, sometimes, irreversible.
However, macular oedema, which is the most common cause of vision loss in diabetics, can occur at any stage of diabetic retinopathy.